Patient Overview
A 41-year-old male presented with progressive swelling in his right lower leg and ankle with considerable difficulty standing and walking, with some pain and joint movement stiffness in that area. Clinical evaluation, along with imaging scans, showed that he had a sizable malignant tumor involving the distal third of the right tibia, which was diagnosed as a high-grade malignant bone tumor. With careful consideration, Dr. Aashish Chaudhary decided to take a limb-salvage approach concerning the tumor’s size, anatomical location, and proximity to the ankle joint. In order to rehabilitate the patient’s limb function, virtual surgical planning was done by the Curewith3D team to ensure adequate surgical margins for oncological safety. Reconstruction was done with autogenous fibular grafting using patient-specific 3D-printed titanium implants.
Virtual Surgical Planning
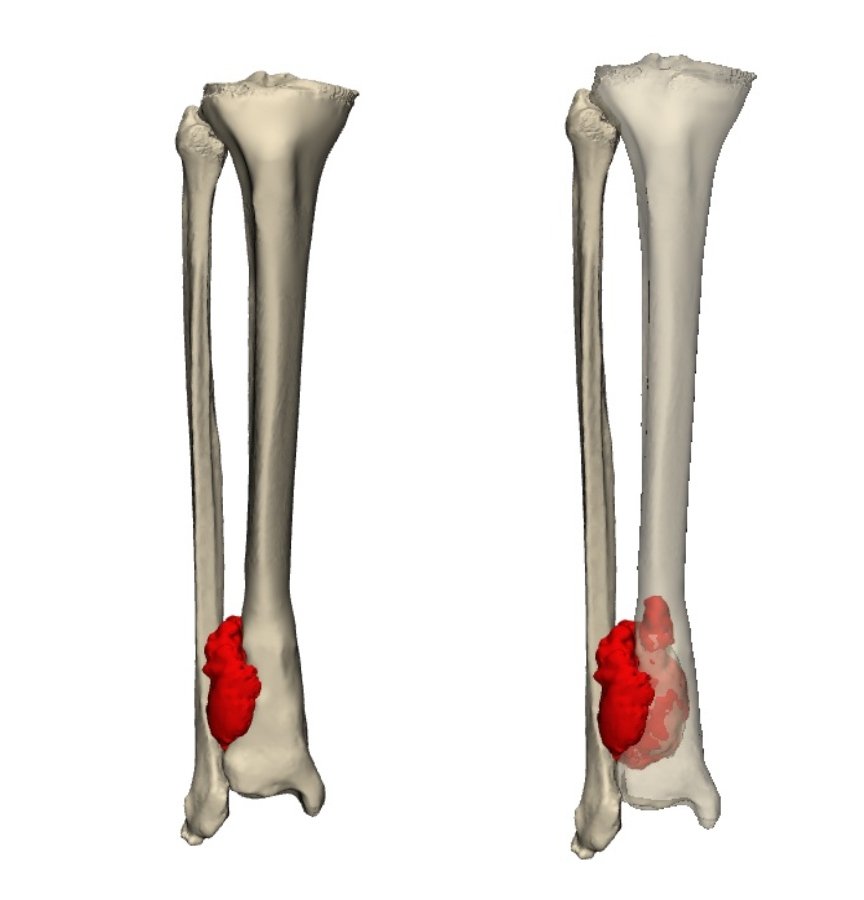
To delineate the full extent of the tumor and plan the resection accurately, a combination of CT and MRI imaging was utilized. The CT scan allowed high-resolution segmentation of the tibial bone, while the MRI provided a clear definition of the tumor’s soft-tissue boundaries. These datasets were digitally fused, enabling the surgical team to visualize the precise transition zone between tumor-infiltrated and healthy bone. This virtual surgical planning (guided by oncologic safety margins) would provide maximum conservation of native bone. The digital simulation also provided a rigid framework for pre-resection reconstruction planning, which is essential for tibia tumor surgery.
3D Modeling of Custom Surgical Guides & Model
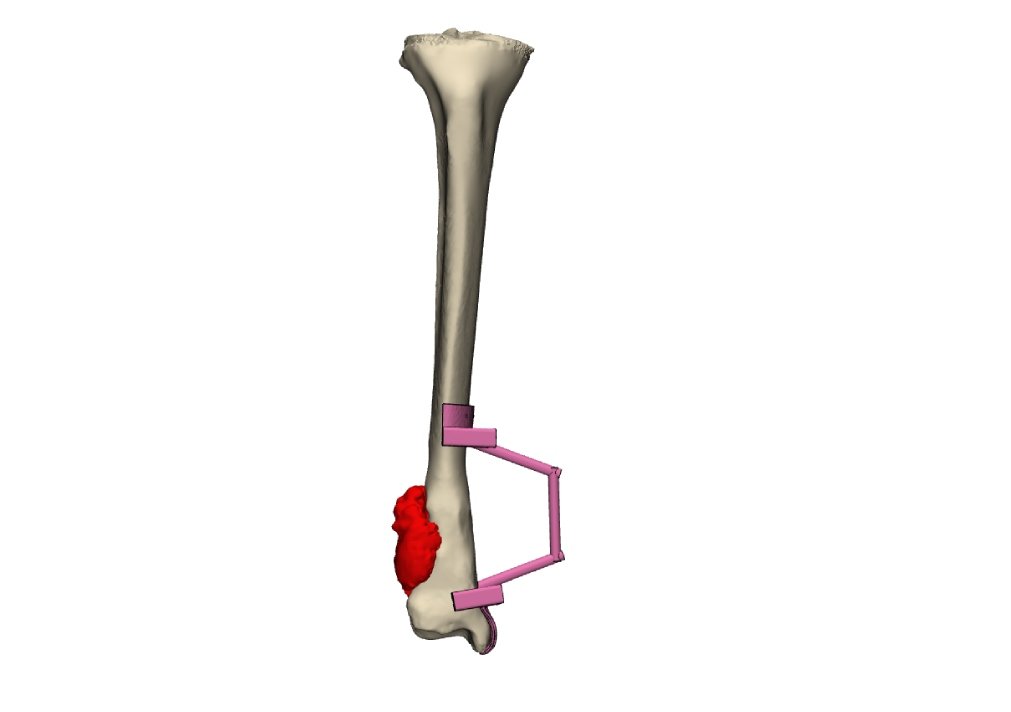
With the imaging data in place, a 3D-printed model of the tumor and distal tibia was created for assessment and preoperative rehearsal. Furthermore, customized orthopedic guides were designed and produced to the precise shape of the patient’s tibia. These guides permitted resection at a millimeter level precision and eliminated intraoperative estimation. The use of 3D technology in the surgery of tumors allowed the surgical team to perform precise excisions with minimal undue trauma to healthy tissues.
Patient-Specific Implant Design
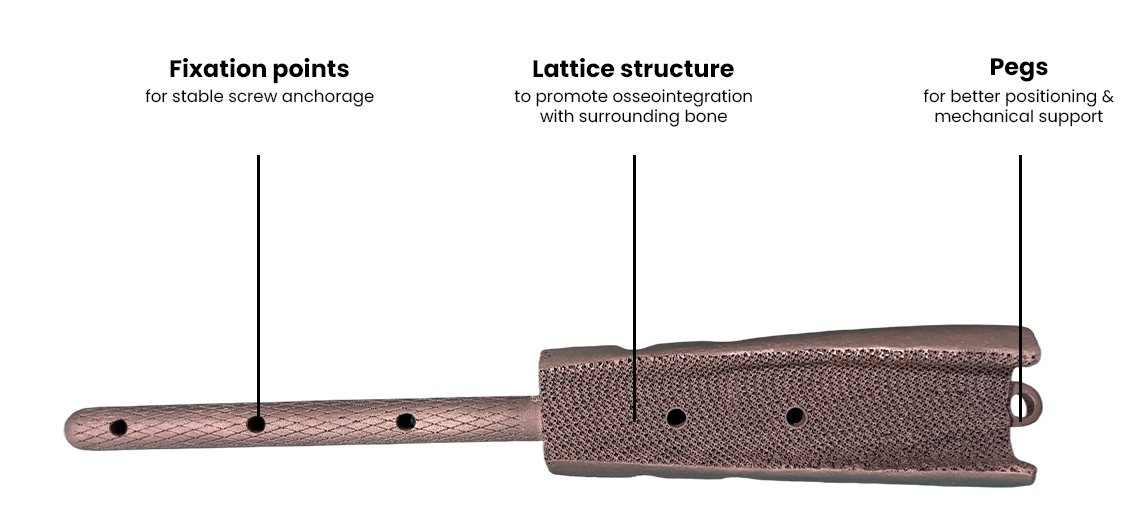
Following the virtual resection, the next phase involved reconstructing the defect with a custom orthopedic implant. For each patient, a patient-specific implant (PSI) was designed and produced in Ti6Al4V titanium alloy. This titanium alloy is recognized for its overall strength, high durability, superior biocompatibility & osteointegration properties. These features, in combination with the anatomical contours of the implant, replicated the patient’s resected tibia.
Patient-specific implants (PSI) include fixation holes, alignment pegs (to reduce the potential for loosening after implant surgery), and a porous lattice structure to facilitate bone ingrowth and long-term biological fixation and reduce the overall weight of the patient-specific implant of the tibia.
Surgical Execution and Fibula Graft Reconstruction
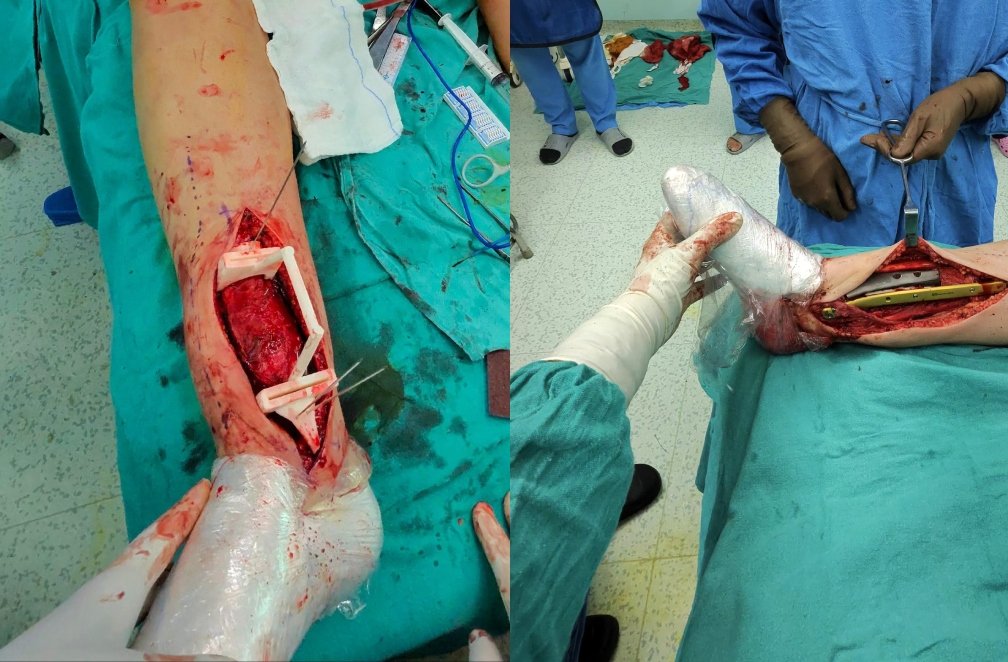
With the imaging data in place, a 3D-printed model of the tumor and distal tibia was created for assessment and preoperative rehearsal. Furthermore, customized orthopedic guides were designed and produced to the precise shape of the patient’s tibia. These guides permitted resection at a millimeter level precision and eliminated intraoperative estimation. The use of 3D technology in the surgery of tumors allowed the surgical team to perform precise excisions with minimal undue trauma to healthy tissues.
Postoperative Recovery and Outcome

Preoperatively, the patient was not able to stand due to pain and instability. He was started on rehabilitative therapy postoperatively and could bear weight partially within weeks. He is now in the process of walking, and imaging scans have shown further osseointegration of the implant and incorporation of the fibular graft. Restoration reconstruction not only restored the anatomic alignment but also the functional mobility, providing the patients better quality of life.